New
Topical Rapamycin: Could This Be Vitiligo’s Next Big Breakthrough?
Vitiligo isn’t just about skin. For the millions worldwide who live with it, the condition often brings a complicated mix of visible changes, social challenges, and daily emotional weight. Over the past decade, treatments have improved—from the old standbys of corticosteroids and phototherapy to the arrival of JAK inhibitors like Opzelura®. But for many, the quest for something safer, longer‑lasting, and more reliable continues.
One of the newest contenders making waves is topical rapamycin, also known as sirolimus or rapamune. Though best known as a immunosuppresant drug used after organ transplants, rapamycin is now being studied as a skin‑applied therapy for vitiligo, with early research suggesting it might help both stop depigmentation and spark repigmentation.
But to understand its promise, it helps to look back at where rapamycin came from and how it’s already reshaping fields far beyond dermatology.
A Journey from Easter Island Soil to Modern Medicine
Rapamycin’s story begins in the 1960s on Easter Island (Rapa Nui), where Canadian researchers collected soil samples during a scientific expedition.(1,2) From these samples, scientists at Ayerst Pharmaceuticals in Montreal isolated a bacterium, Streptomyces hygroscopicus, that secreted a compound with striking antifungal activity. They named it rapamycin, after the island’s indigenous name. What started as an antifungal discovery quickly grew in scope: rapamycin was later found to be a potent immunosuppressant and anti-cancer agent. More importantly, it inhibits mTOR (mechanistic Target of Rapamycin) — a master regulator of cell growth, metabolism, and immune function — making it one of the most influential molecules in modern biomedical research.
How Rapamycin Works
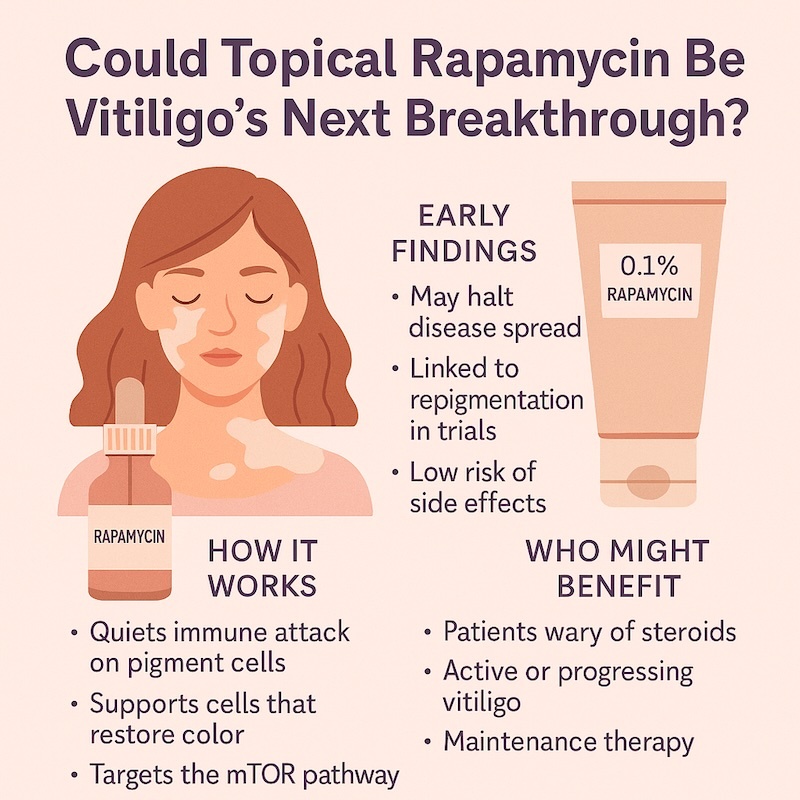
Unlike corticosteroids and JAK inhibitors, rapamycin targets the mTOR pathway — a key regulator of cell growth, metabolism, and immune system activity. In vitiligo, overactive immune responses attack melanocytes, the pigment‑producing cells. Rapmycin doesn’t just quiet specific immune signals; it helps recalibrate the entire cellular environment where melanocytes — the pigment-producing cells — live and work. Early data suggest rapamycin may both suppress the autoimmune destruction of melanocytes and create conditions that allow these cells to regenerate and repopulate depigmented patches.(1)
Rapamycin and Longevity: Lessons from a Different Field
It might sound counterintuitive that an immunosuppressant like rapamycin could improve immune function — but that’s exactly what some researchers believe. The key lies in dosage and context.
In transplant or cancer settings, patients take rapamycin at high doses, effectively shutting down the mTOR pathway to dampen immune responses. But aging brings a different challenge: as we get older, the mTOR pathway tends to become overactive. Instead of turning it off, the goal becomes turning it down—restoring it to more “youthful” levels.
In this light, low-dose, intermittent rapamycin acts less like a blunt tool and more like a cellular tuner. Animal studies show that it can extend lifespan, reduce cancer risk, and improve function across organs — immune system included. In humans, early trials suggest similar benefits: older adults given low-dose rapamycin show improved immune responses to vaccines and better overall resilience, though large-scale studies are still underway.
This dual identity — as both immune suppressor and immune optimizer — adds nuance to rapamycin’s promise in dermatology. It’s not just about symptom control. If topical rapamycin helps modulate mTOR activity in the skin, it could reset some of the cellular dysfunctions at the heart of vitiligo in ways that current treatments don’t address.
Where We Stand in Vitiligo Research
So far, rapamycin hasn’t been approved for vitiligo anywhere in the world, but momentum is building.
An ongoing Phase II clinical trial (NCT05342519) is testing daily topical rapamycin at two concentrations (0.1% and 0.001%) on patients with nonsegmental vitiligo. Each participant applies rapamycin to one lesion and a placebo to a matched lesion on the other side, for six months. Interim insights and related research suggest rapamycin is well‑tolerated, with most side effects limited to mild, temporary skin irritation. Systemic absorption appears minimal, which is encouraging given rapamycin’s known risks when taken orally.
Early Takeaways
So far, the story looks cautiously promising. Preliminary reports suggest:
- Disease control: Rapamycin may help “switch off” the ongoing immune attack that fuels active vitiligo.
- Pigment return: Daily application has been linked to gradual repigmentation in early cases.
- Good tolerability: Side effects have mostly been limited to mild redness or irritation, with virtually no systemic absorption detected.
How It’s Being Used in Trials
Most studies test ointments or gels containing either 0.1% or 0.001% rapamycin, applied once daily for several months. Some protocols stretch to a year. Researchers are also exploring how rapamycin pairs with other mainstays like narrowband UVB phototherapy—though we don’t yet know the best recipe for combining them.
One important caveat: rapamycin cream isn’t something patients should try to whip up at home. It requires precise compounding and careful monitoring by a dermatologist.
Who Might Benefit Most
- Patients wary of steroids or JAK inhibitors: Rapamycin may offer a lower‑risk alternative.
- Those with active or spreading vitiligo: Its immune‑modulating effect could help stop the spread.
- Maintenance therapy seekers: In time, rapamycin might play a role in keeping repigmentation gains after other treatments.
The Road Ahead
The dermatology world is waiting for answers from larger trials expected in 2026. These will clarify not just how well rapamycin works, but how best to use it — what dose, how long, and whether it pairs well with phototherapy or other drugs.
If the data come through, rapamycin could become a welcome addition to the vitiligo treatment toolkit—one that’s gentler than many current options but still effective at restoring confidence and color.
The Safety Ledger
Like any powerful substance, rapamycin comes with caveats. At higher systemic doses, it can raise infection risk, slow wound healing, and trigger metabolic issues such as elevated cholesterol, blood sugar, or even type 2 diabetes. Other side effects may include mouth ulcers, rashes, and swelling.(1) In anti-aging trials, scientists often use low, intermittent dosing to minimize risks — a strategy that may also shape dermatology protocols if topical rapamycin gains traction.
Final Thought
Nature didn’t design rapamycin to treat vitiligo — or aging, or cancer, for that matter. But after millions of years of microbial evolution, it came remarkably close. Now, the real challenge is refinement: how to keep its powerful effects on mTOR while dialing back the downsides.
That’s exactly what a new wave of researchers is working on — developing next-gen compounds that preserve rapamycin’s benefits without the immune suppression baggage. If they succeed, we won’t just have a better drug. We might have a whole new class of tools for treating chronic disease — and reshaping what long-term health looks like.
— Yan Valle
Professor h.c., CEO VR Foundation | Author, A No-Nonsense Guide to Vitiligo
Dig deeper:
- Acral Vitiligo and Platelet-Rich Plasma: Your Questions Answered
- Ayahuasca as a Potential Therapy for Vitiligo. A Journey into the Mind-Body Connection
- Diet, Microbiome, and Vitiligo: Unveiling the Mystery
FAQOther Questions
- How to get insurance coverage for vitiligo treatments?
Getting insurance coverage for vitiligo treatments can be challenging, but there are several steps you can take to improve your chances For a more in-depth look, check out our ...
- How long does it take to treat vitiligo?
Vitiligo, a condition characterized by the loss of skin pigment, can be unpredictable in both progression and treatment. The time it takes to treat vitiligo varies significantly...
- PTSD in Vitiligo?
Living with vitiligo often involves more than managing visible skin changes. Many individuals face discrimination, social stigma, and feelings of isolation, leading to emotional...
Though it is not always easy to treat vitiligo, there is much to be gained by clearly understanding the diagnosis, the future implications, treatment options and their outcomes.
Many people deal with vitiligo while remaining in the public eye, maintaining a positive outlook, and having a successful career.
Copyright (C) Bodolóczki JúliaBy taking a little time to fill in the anonymous questionnaire, you can help researchers better understand and fight vitiligo.
